By: Alfonso C. Hernandez-Romieu, MD; Serena Leung, MPH; Armand Mbanya, MD; Brendan R. Jackson, MD; Jennifer R. Cope, MD; Dena Bushman, MSN, MPH; Meredith Dixon, MD; Jessica Brown, PhD; Tim McLeod, MPH; Sharon Saydah, PhD; Deblina Datta, MD; Kate Koplan, MD; Felipe Lobelo, MD, PhD
Published April 30, 2021
CDC
Health care needs in the months after a COVID-19 diagnosis among nonhospitalized adults have not been well studied.
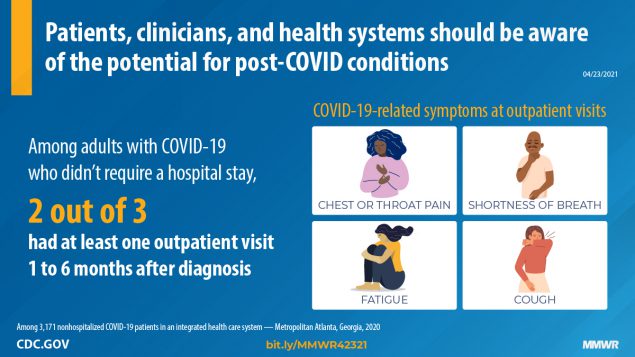
Among 3,171 nonhospitalized adult COVID-19 patients, 69% had one or more outpatient visits 28–180 days after the diagnosis. Two thirds had a visit for a new primary diagnosis, and approximately one third had a new specialist visit. Symptoms potentially related to COVID-19 were common new visit diagnoses. Visits for these symptoms decreased after 60 days but for some patients continued through 120–180 days.
Clinicians and health care systems should be aware of the potential for post-COVID conditions.
As of April 19, 2021, 21.6 million COVID-19 cases had been reported among U.S. adults, most of whom had mild or moderate disease that did not require hospitalization. Health care needs in the months after COVID-19 diagnosis among nonhospitalized adults have not been well studied. To better understand longer-term health care utilization and clinical characteristics of nonhospitalized adults after COVID-19 diagnosis, CDC and Kaiser Permanente Georgia (KPGA) analyzed electronic health record (EHR) data from health care visits in the 28–180 days after a diagnosis of COVID-19 at an integrated health care system. Among 3,171 nonhospitalized adults who had COVID-19, 69% had one or more outpatient visits during the follow-up period of 28–180-days. Compared with patients without an outpatient visit, a higher percentage of those who did have an outpatient visit were aged ≥50 years, were women, were non-Hispanic Black, and had underlying health conditions. Among adults with outpatient visits, 68% had a visit for a new primary diagnosis, and 38% had a new specialist visit. Active COVID-19 diagnoses (10%) and symptoms potentially related to COVID-19 (3%–7%) were among the top 20 new visit diagnoses; rates of visits for these diagnoses declined from 2–24 visits per 10,000 person-days 28–59 days after COVID-19 diagnosis to 1–4 visits per 10,000 person-days 120–180 days after diagnosis. The presence of diagnoses of COVID-19 and related symptoms in the 28–180 days following acute illness suggests that some nonhospitalized adults, including those with asymptomatic or mild acute illness, likely have continued health care needs months after diagnosis. Clinicians and health systems should be aware of post-COVID conditions among patients who are not initially hospitalized for acute COVID-19 disease.
Patients aged ≥18 years who received positive results for SARS-CoV-2 (the virus that causes COVID-19) by polymerase chain reaction testing performed during April 4–September 17, 2020, and for whom ≥180 days had elapsed since their testing date were identified in KPGA EHR data. Patients were not included in the analysis if they were hospitalized in the 28 days after COVID-19 diagnosis, were pregnant during the 12 months before or at the time of COVID-19 diagnosis, or were not continuously enrolled in KPGA during the year preceding COVID-19 diagnosis. Among 3,171 patients included in the analysis, health care utilization and International Classification of Diseases, Tenth Revision (ICD-10) diagnostic codes were obtained for outpatient (i.e., clinic or urgent care) and emergency department visits, and hospitalizations occurring 28–180 days after COVID-19 diagnosis.
Health care utilization was determined based on the number, type (i.e., video, telephone, and in-person), setting (i.e., clinic, urgent care, emergency department, and hospital), and clinical specialty of visits. New specialty visits were defined as specialists that a patient had not consulted in the 12 months preceding COVID-19 diagnosis. New specialty visits were classified as potentially related to COVID-19 based on previously described multiorgan effects in post-COVID conditions (2). Clinical characteristics were ascertained through active primary and secondary ICD-10 codes for outpatient visits. ICD-10 codes were classified as new diagnoses if they had not been documented in the 12 months preceding COVID-19 diagnosis; otherwise, they were classified as preexisting conditions. Administrative ICD-10 codes were classified as “other.” Primary diagnoses were used to classify visit type as being for a new or preexisting condition or other. Primary and secondary diagnoses were used to describe common visits diagnoses and were classified as COVID-19–related, potentially COVID-19–related, new, or preexisting. All health care utilization and clinical characteristics were described at 28–59, 60–119, and 120–180 days after COVID-19 diagnosis. Diagnoses were described as diagnosis-specific visit rates (visits per 10,000 person-days). Continuous variables were compared using t-tests or Wilcoxon signed-rank tests, and proportions were compared using chi-square or Fisher’s exact tests, as required. SAS (version 9.4; SAS Institute) was used to perform statistical analyses. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.
Among 3,171 identified adults with COVID-19, a total of 2,177 (69%) had one or more outpatient visits 28–180 days after COVID-19 diagnosis. The proportion of adults with one or more visits was significantly higher among adults aged ≥65 years (88%) than among those aged 18–49 years (66%), among women (76%) than among men (59%), among non-Hispanic Black adults (71%) than among all others (68%) (p = 0.04), and among adults with three or more underlying health conditions (83%) than among those with no (60%) or one or two (69%) underlying conditions.
Among adults with one or more outpatient visits, 7,991 visits occurred 28–180 days after COVID-19 diagnosis, with a median of two (interquartile range = 1–4) visits per patient. Fewer than 2% (32) of patients were hospitalized 28–180 days after COVID-19 diagnosis. More than two thirds of patients (1,617; 68%) had visits for a new primary diagnosis. Among specialists visited, 1,627 (75%) patients visited a family, geriatric, or internal medicine provider, and 823 (38%) visited with a new specialist. Common new specialty visits potentially related to COVID-19 included dermatology (16%), behavioral/mental health (11%), gastroenterology (11%), and cardiology (10%). Overall, 58 (3%) patients saw a pulmonologist; 41 (71%) of these patients had not been evaluated by this specialty in the 12 months preceding their COVID-19 diagnosis.
COVID-19 was recorded as an active diagnosis for 210 (10%) of 2,177 patients who had one or more outpatient visit within 180 days of COVID-19 diagnosis. COVID-19–related visits declined from 24 per 10,000 person-days during the 28–59-day interval to fewer than two per 10,000 person-days during the 120–180-day interval. Visits per 10,000 person-days for symptoms potentially related to COVID-19 declined during these same intervals, including those for throat or chest pain (from seven per 10,000 person-days to four), shortness of breath (from eight to three), cough (from four to two), and malaise and fatigue (from four to two). In contrast, rates of visits with chronic disease diagnoses (e.g., hypertension and diabetes) and urinary tract infections changed little over time.
0 Comments