By: Hanna B. Demeke, PhD; Sharifa Merali, MPH; Suzanne Marks, MPH, MA; Leah Zilversmit Pao, PhD; Lisa Romero, DrPH; Paramjit Sandhu, MD; Hollie Clark, MPH; Alexey Clara, MD; Kendra B. McDow, MD; Erica Tindall, MSN, MPH; Stephanie Campbell, MPH; Joshua Bolton, MS; Xuan Le, AM; Julia L. Skapik, MD; Isaac Nwaise, PhD; Michelle A. Rose, PhD; Frank V. Strona, MPH; Christina Nelson, MD; Charlene Siza, DVM
Published February 19, 2021
CDC
Telehealth can facilitate access to care, reduce risk for transmission of SARS-CoV-2, conserve scarce medical supplies, and reduce strain on health care capacity and facilities while supporting continuity of care.
Telehealth can facilitate access to care, reduce risk for transmission of SARS-CoV-2 (the virus that causes coronavirus disease 2019 [COVID-19]), conserve scarce medical supplies, and reduce strain on health care capacity and facilities while supporting continuity of care. Health Resources and Services Administration (HRSA)–funded health centers expanded telehealth services during the COVID-19 pandemic. The Centers for Medicare & Medicaid Services eliminated geographic restrictions and enhanced reimbursement so that telehealth services–enabled health centers could expand telehealth services and continue providing care during the pandemic. CDC and HRSA analyzed data from 245 health centers that completed a voluntary weekly HRSA Health Center COVID-19 Survey for 20 consecutive weeks to describe trends in telehealth use. During the weeks ending June 26–November 6, 2020, the overall percentage of weekly health care visits conducted via telehealth (telehealth visits) decreased by 25%, from 35.8% during the week ending June 26 to 26.9% for the week ending November 6, averaging 30.2% over the study period. Weekly telehealth visits declined when COVID-19 cases were decreasing and plateaued as cases were increasing. Health centers in the South and in rural areas consistently reported the lowest average percentage of weekly telehealth visits over the 20 weeks, compared with health centers in other regions and urban areas. As the COVID-19 pandemic continues, maintaining and expanding telehealth services will be critical to ensuring access to care while limiting exposure to SARS-CoV-2.
In April 2020, HRSA began administering a voluntary weekly Health Center COVID-19 Survey to track the effect of COVID-19 on health centers’ testing capacity, operations, patients, and staff members. Potential respondents were 1,382 HRSA-funded health centers. CDC and HRSA analyzed data from 245 health centers that responded to the Health Center COVID-19 Survey for 20 consecutive weeks (weeks ending June 26–November 6, 2020) to examine trends in telehealth use, assess differences by U.S. Census region and urbanicity, and compare telehealth patterns with the 7-day average number of new known COVID-19 cases within the counties where the included health centers were located. Region and urbanicity have previously been shown to be strongly associated with telehealth use (1). Each health center recorded the percentage of weekly telehealth visits in intervals of five (range = 0–100). Compared with health centers that responded at least once to the Health Center COVID-19 Survey over the study period (range = 912–1,011), consecutively responding health centers were more often located in more urban geographic areas (62.9% versus 58.5%) and in the Northeast (20.4% versus 16.7%) and West (29.4% versus 27.1%) regions than were those that did not report consecutively.
The average percentage of weekly telehealth visits was calculated nationally by region, and by urbanicity. Overall and weekly changes in telehealth visits (absolute percentage point difference and percentage change) for the first 10 weeks (weeks ending June 26–August 28, 2020) and the second 10 weeks (weeks ending September 4–November 6, 2020) were calculated. Weekly changes were calculated as the average of week-to-week differences in weekly telehealth visits for the first and second 10 weeks of the study period. The Kruskal-Wallis test was used to measure differences in the overall average percentage of weekly telehealth visits by region and urbanicity. Post hoc tests for pairwise comparisons were conducted if the Kruskal-Wallis test identified a significant main effect. P-values <0.05 were considered statistically significant. The 7-day average number of new known COVID-19 cases from 210 counties where the 245 health centers were located was accessed from USAFacts and calculated for each week of the survey and compared with the average percentage of weekly telehealth visits nationally by region and urbanicity. SPSS Statistics software (version 20; IBM) was used to conduct all analyses. These activities were reviewed by CDC and were conducted consistent with applicable federal law and CDC policy.
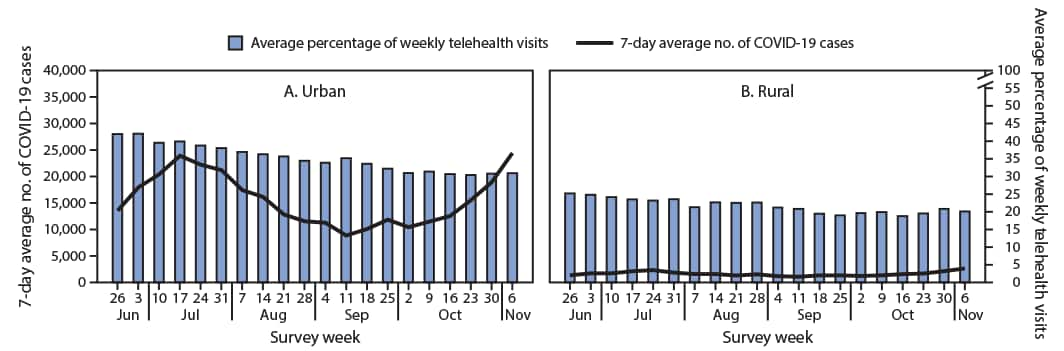
The overall average percentage of weekly telehealth visits among 245 consecutively responding health centers decreased 25%, from 35.8% during the week ending June 26, to 26.9% for the week ending November 6, averaging 30.2% over the study period. Health centers in the South census regions and rural areas reported the lowest average percentage of weekly telehealth visits compared with health centers in other census regions and urban areas. During the first 10 weeks of study (June 26–August 28), health centers in the Northeast reported the largest absolute change in average percentage of weekly telehealth visits (–13.3%) followed by health centers in the Midwest (–7.3%). Urban health centers reported a larger absolute change in percentage of weekly telehealth visits for both the first 10 weeks (–7.6%) and the second 10 weeks of study (–3.0) compared with the change in rural health centers (–2.6% and –1.1%, respectively). Health centers in the Northeast reported stable weekly telehealth visits, with an absolute change of 0.1% over the second 10 weeks of study (September 4–November 6). Within each region and urbanicity stratum, the overall change in average percentage of telehealth visits differed significantly between the first 10 weeks and the last 10 weeks of the study period.
The overall average percentage of weekly telehealth visits differed significantly among some regions. Pairwise comparisons found that the overall average percentage in the South was significantly lower than that in the Northeast (p<0.01) and the West (p<0.01). The percentages of telehealth visits in the Northeast and the West did not differ significantly (p = 0.793). Urban health centers reported a significantly higher overall average percentage of telehealth visits than did rural health centers (p<0.01). The number of COVID-19 cases varied by region and increased overall during the second half of the study period (Figure 1). The increase in COVID-19 cases in the Northeast in the second 10 weeks of the study period aligned with the plateauing and slightly increasing trend in average percentage of weekly telehealth visits. The number of COVID-19 cases in the counties where urban health centers were located peaked in the week ending July 4 in the first 10 weeks and consistently increased in the second 10 weeks (Figure 2). However, the average percentage of weekly telehealth visits continued to trend downward.
0 Comments